
11 events to accompany Smithsonian exhibition in Essex | News | gloucestertimes.com Gloucester Daily Times

11 events to accompany Smithsonian exhibition in Essex | News | gloucestertimes.com Gloucester Daily Times
Reports & Events Monthly Calendar – September 2022 The National Academies of Sciences, Engineering, and Medicine

Perioperative respiratory adverse events (PRAEs) are often seen in children after they get an adenotonsillectomy (AT), one of the most common procedures children receive worldwide. ATs are performed for treating sleep-disordered breathing and obstructive sleep apnea syndrome (OSAS). In a recent study, investigators tested for causes of perioperative respiratory adverse events (PRAEs) in children. The goal of the study was to control factors which lead to respiratory complications.
Benzodiazepine midazolam is the most frequent form of preoperative pharmacologic anxiolysis given to children, though recently α-2 agonist dexmedetomidine has been equally common. These are intranasal formulations, allowing children to take them without intravenous access. However, these medicines, along with analgesics such as opioids and anesthetics, may make PRAEs more likely to appear. This is not certain, as data is inconclusive.
Investigators conducted a clinical trial comparing the appearance of PRAES in 384 children after receiving midazolam, dexmedetomidine, or saline control. The midazolam group had the highest rate of PRAEs at 56.5%, followed by the saline control group at 40.8% and the dexmedetomidine group at 24.2%.
Prior studies indicated that dexmedetomidine and midazolam are similarly effective for anxiolysis, but dexmedetomidine is favorable for preventing emergence delirium. In this study, investigators hypothesized that preoperative midazolam and dexmedetomidine would lead to less PRAEs appearing in children.
Investigators found that PRAEs are 5 times more likely to appear in children with OSAS when they undergo AT. As OSAS also leads to higher sensitivity toward opioids, patients were recommended to be given half of a normal opioid dosing.
The patients in this study were clinically diagnosed with OSAS, and investigators were unsure how accurate these diagnoses were. OSAS diagnoses have been recorded with an accuracy range of 30% to 85%. This led to the patients in the trial possibly having unequal levels of OSAS severity.
At the end of the study, investigators concluded that there was still much complexity surrounding preoperative anxiolytic use, and suggested that all medications be carefully considered in the context of each child’s needs and risks.
Reference
Dalesio NM, Kudchadkar SR. Perioperative respiratory adverse events after pediatric adenotonsillectomy—evaluating the role of preoperative pharmacologic anxiolysis. JAMA Network Open. 2022;5(8):e2225482. doi:10.1001/jamanetworkopen.2022.25482

Experts at the University of Nottingham, in collaboration with experts at Keele University, have found that the risk of heart attacks and strokes temporarily increases in the four months after a gout flare.
The research showed that gout patients who suffered from a heart attack or stroke were twice as likely to have had a gout flare in the 60 days prior to the event, and one and a half times more likely to have a gout flare in the 61-120 days prior.
The results of the study, led by Professor Abhishek in the School of Medicine at the University of Nottingham, are published in the journal JAMA.
Gout is a common form of arthritis that affects one in 40 adults in the UK. It is caused by high levels of uric acid, a chemical produced by breakdown of tissues in the body and present in certain foods and drinks.
At high levels, uric acid is deposited in and around joints as needle shaped urate crystals. Once released from their deposits, these crystals cause severe inflammation manifesting as joint pain, swelling, redness, and tenderness that often lasts for 1-2 weeks. These episodes, called gout flares, often recur. Inflammation is also a risk factor for heart attack and stroke.
People with gout tend to have more cardiovascular risk factors, although there have been no previous studies about whether gout flares are linked with an increased risk of heart attack and stroke. In this study, the experts examined whether there was a temporary increase in risk of heart attack or stroke after a gout flare.
The team used anonymized data from 62,574 patients with gout treated in the National Health Service in the UK. Of these, 10,475 experienced heart attack or stroke after the diagnosis of gout, while others of similar age, sex, and duration of gout, did not experience such events. They evaluated the association between heart attacks or strokes and recent gout flares and adjusted these results for comorbidities, socioeconomic deprivation, lifestyle factors and prescribed medications among other things. They found that gout patients who suffered a heart attack or stroke were twice as likely to have had a gout flare in the 60 days prior to the event, and one and a half times more likely to have a gout flare in the preceding 61-120 days.
They found a similar high rate of heart attack or stroke in the 0-60 and 61-120 days after gout flares compared with other time periods, when they used information from only patients who consulted for a gout flare and also experienced either heart attack or stroke. This further strengthened the finding that gout flares are associated with a transient increase in cardiovascular events following flares. The increased odds and rates persisted when people with pre-existing heart disease or stroke before their gout diagnosis were excluded, and when shorter exposure periods such as 0-15 and 16-30 days prior to heart attack or stroke, were considered.
Gout patients who died from a heart attack or stroke had over four times the odds of experiencing a gout flare in the preceding 0-60 days and over twice the odds of gout flare in the preceding 61-120 days.
This is the first study of its kind to examine whether there is an association between recent gout flares and heart attacks and strokes.
The results show that among patients with gout, patients who experienced a heart attack or stroke had significantly increased odds of a gout flare during the preceding 120-days compared with patients who did not experience such events. These findings suggest that gout flares are associated with a transient increase in cardiovascular events following flares.
People with recurrent gout flares should be considered for long-term treatment with urate lowering treatments such as allopurinol. This is a reliable way of removing urate crystal deposits and providing freedom from gout flares. Patients should also be considered for concurrent treatment with anti-inflammatory medicines such as colchicine for the first few months because urate lowering treatments may trigger gout flares in the short term.
People with gout should be encouraged to adopt a healthy lifestyle with appropriate treatment of conditions such as high blood pressure, high cholesterol, obesity and diabetes to minimise their background risk of heart attack and stroke”
Professor Abhishek, lead author on the study
Source:
Journal reference:
Cipolletta, E., et al. (2022) Association Between Gout Flare and Subsequent Cardiovascular Events Among Patients With Gout. JAMA. doi.org/10.1001/jama.2022.11390.

The annual Medicine Hat Stampede is back with events, food, live entertainment, and activities you love!
One of the most anticipated events of the summer, Stampede Week is July 27 through July 30, with the official kick off parade happening downtown on Thursday, July 28. As far as live entertainment this year, you can look forward to seeing Trace Adkins, Mackenzie Porter and The Beach Boys performing the Night Shows.
The Midway will be back in full this year with games, rides and, of course, the mini donuts everyone waits all year for! Mark your calendars for a fun-filled week for the whole family.
Stampede tickets are free when you buy a Night Show or Rodeo ticket by Tuesday, July 26! More information about the Medicine Hat Stampede can be found on their website.
3. Heritage Gather Festival
From August 5-7, Dunmore Equestrian Society and Rugged Rodeo Inc. presents the Heritage Gather Festival, a weekend celebration of Indigenous Culture and Western Heritage! The inclusive, family-friendly festival will host a variety of traditional events, from Open Rodeo, to Ranch Bronc Riding, Indian Relay Race Demos, and Powwow, along with many more! Find the full schedule of events from Friday to Sunday here.
4. Miywasin Story Tour
The second Miywasin Story Tour of the year is happening on Saturday, August 20! It is described as ‘an integral part of the preservation and expression of culture in Indigenous communities’ and includes a guided tour of key Indigenous areas in Medicine Hat: Saamis Tepee, Saamis Archaeological Site, and the Métis Community in Saratoga Park.
Transportation on the Sunshine Trolley is provided with pick-up and drop-off at the Miywasin Friendship Centre downtown. There is opportunity for a traditional Indigenous hands-on activity.
To reserve your spot, Miywasin Story Tour tickets can be purchased here.
5. Battle Creek Showdown Mountain Bike Race
On Saturday, August 27th, the Battle Creek Showdown Mountain Bike Race is happening! The event is taking place in Elkwater and will feature bike races, live music and tons of food! Take your family just outside of Medicine Hat for an epic weekend of fun.
More information about the event can be found on their Facebook page.
Reports & Events Monthly Calendar – July 2022 The National Academies of Sciences, Engineering, and Medicine
Upcoming events surrounding the Hat Medicine Hat News
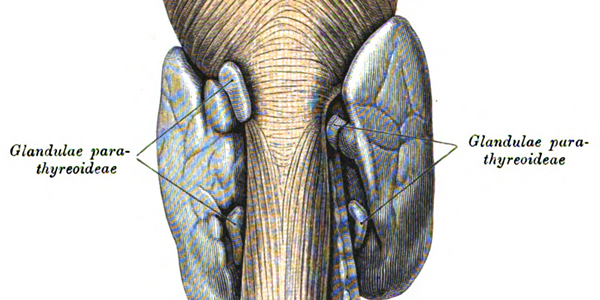
1. In this cohort study, among 16 374 Swedish adult patients with primary hyperparathyroidism, the risk hip fracture was increased by 51%, and risk of cardiovascular events increased by 45% compared to matched healthy participants.
2. Parathyroidectomy was associated with a reduced risk of any fracture, hip fracture, cardiovascular events and death.
Evidence Rating Level: 2 (Good)
Study Rundown: Primary hyperparathyroidism (pHPT) is an endocrine disorder in which individuals have an elevated serum calcium combined with a normal or high blood level of parathyroid hormone. Known concerns of pHPT include increased bone loss and an elevated risk of fractures at sites including the spine, wrist, ribs and pelvis. As such, this retrospective cohort study investigated whether untreated pHPT was associated with an increased risk of fractures and cardiovascular events (CVEs) in comparison with the risk of a sex, age and country-matched control group and whether parathyroidectomy was associated with a reduction in these outcomes. The study included patients who were diagnosed with pHPT at hospitals in Sweden between 2006 to 2017. The primary outcomes were fractures, CVEs, and death. A total of 16 374 patients with pHPT were identified with a mean age of 67.5 years. Compared with the control group, the pHPT group was found to have a higher risk of any fracture by 39%, hip fracture by 51%, CVEs 45% and death 72%. Parathyroidectomy was associated with a reduced risk of any fracture by 17% and death by 59%. A major strength of this study was that in terms of the number of patients with untreated pHPT and multiple observed outcomes, it is the largest analysis performed thus far. As a result of the observational design however, a limitation to this study is that it could not establish causality, although the time-dependent analysis suggested an association between parathyroidectomy and reduced risk of fractures, CVEs and death.
Click to read the study in JAMA Network Open
Relevant Reading: Survival after the diagnosis of primary hyperparathyroidism: a population-based study
In-Depth [retrospective cohort]: This study investigated whether primary hyperparathyroidism (pHPT) was associated with an increased risk of fractures, CVEs and mortality, compared to the risk of a sex, age and country-matched control group. Data was collected from patients diagnosed with pHPT at hospitals in Sweden between July 1, 2006 to December 31, 2017. Each patient was matched with 10 control individuals from the general population. A total of 16 374 patients with pHPT were identified (mean SD age, 67.5 [12.9] years; 12806 women [78.2%]), with 163 740 control individuals. The median follow-up time for the pHPT group was 1.15 (.040-4.06) years and for the control it was 4.62 (2.08-7.51) years. Patients with pHPT had significantly higher risks of any fracture (unadjusted HR, 1.39; 95% CI, 1.31-1.48), major osteoporotic fracture (unadjusted HR, 1.43; 95% CI, 1.33-1.54), hip fracture (unadjusted HR, 1.51; 95% CI, 1.35-1.70), and injurious fall (unadjusted HR, 1.51; 95% CI, 1.42-1.60) compared with those in the control group. The risk of fractures was significantly increased at the following sites: wrist (unadjusted HR, 1.34; 95 CI, 1.18-1.52), upper arm (unadjusted HR, 1.46; 95% CI, 1.25-1.71) and lower leg (unadjusted HR, 1.31; 95% CI, 1.12-1.54). The risk of any CVE for patients with pHPT was increased (unadjusted HR, 1.45; 95% CI, 1.34-1.57), as well as the risk for acute myocardial infarction (unadjusted HR, 1.39; 95% CI, 1.24-1.56) and ischemic stroke (unadjusted HR, 1.51; 95%CI, 1.36-1.68). The risk of death (unadjusted HR, 1.72; 95% CI, 1.65-1.80) was also increased in higher in patients with pHPT compared to the control group. There was a substantial increase in the risk of kidney stones, almost 4 times higher in patients with pHPT (unadjusted HR, 3.65; 95% CI, 3.27-4.08) than in control individuals. Of the 16 374 patients with pHPT, 6934 (42.3%) underwent a parathyroidectomy. While using the Poisson regression model to study the pHPT group separately, parathyroidectomy was found to be associated with a reduced risk of hip fracture (HR, 0.78; 95% CI, 0.61-0.98), any fracture (HR, 0.83; 95% CI, 0.75-0.93), injurious fall (HR, 0.83; 95% CI, 0.74-0.92), CVE (HR, 0.84; 95% CI, 0.73-0.97), and death (HR, 0.59; 95% CI, 0.53-0.65).
Image: PD
©2022 2 Minute Medicine, Inc. All rights reserved. No works may be reproduced without expressed written consent from 2 Minute Medicine, Inc. Inquire about licensing here. No article should be construed as medical advice and is not intended as such by the authors or by 2 Minute Medicine, Inc.
Results from a real-world study investigating safety and effectiveness of clopidogrel versus aspirin monotherapy beyond 12 months after PCI in high-risk patients during the chronic maintenance period. This study found that clopidogrel monotherapy was associated with reduced risk of net adverse clinical events (NACE; all-cause death, MI, stent thrombosis, stroke, or BARC type 2, 3, or 5 bleeding) and MACCE (death, MI, stent thrombosis, stroke), and a numerical decrease in major or clinically relevant nonmajor bleeding (BARC type 2, 3, or 5 bleeding), compared with aspirin monotherapy. The findings were presented today as late-breaking clinical research at the Society for Cardiovascular Angiography & Interventions (SCAI) 2022 Scientific Sessions.
P2Y12 inhibitor monotherapy reduces bleeding risk without increasing the risk of ischemic events compared with dual antiplatelet therapy (DAPT), especially in the first 12 months following percutaneous coronary intervention (PCI). Recent research showed that among patients who were event free for six to 18 months post-PCI and successfully received the intended duration of DAPT, clopidogrel monotherapy was superior compared with aspirin monotherapy in terms of NACE. However, optimal antiplatelet monotherapy during the chronic maintenance period beyond 12 months after PCI with drug-eluting stents in high-risk patients in real-world settings is previously unknown.
In total, 8,377 consecutive patients at high risk for both bleeding and thrombosis were identified from the prospective Fuwai PCI Registry if they satisfied one clinical and one angiographic criterion. Patients who received antiplatelet (aspirin or clopidogrel) monotherapy longer than 12 months and were free from ischemic and bleeding events at 12-month post-PCI without extended duration of DAPT were included. The primary endpoint was net adverse clinical events (NACE) from 12 to 30 months. The key secondary endpoints were major adverse cardiac or cerebral events (MACCE) and major or clinically relevant nonmajor bleeding (BARC type 2, 3 or 5).
“These findings show for the first time clopidogrel monotherapy is associated with reduced risk of long-term NACE and MACCE,” said Hao-Yu Wang, Cardiometabolic Medicine Center, Coronary Heart Disease Center, Department of Cardiology, Fuwai Hospital, State Key Laboratory of Cardiovascular Disease, National Center for Cardiovascular Diseases, Chinese Academy of Medical Sciences and Peking Union Medical College, Beijing, China. “Our results may have important practical implications for determining the optimal treatment for patients requiring a single antiplatelet drug, either aspirin or clopidogrel, for secondary prevention of ischemic events in high-risk PCI population.”
Of 7,392 high-risk patients that were event-free after the first year and adherent to DAPT, 5,664 patients who received antiplatelet monotherapy (clopidogrel monotherapy: n=1,974 and aspirin monotherapy: n=3690) were included in the present analysis. Researchers found that between 12 and 30 months, the net adverse clinical events were lower with clopidogrel monotherapy compared to aspirin monotherapy (Kaplan-Meier estimate: 2.5% vs. 5.0%; adjusted HR:0.566, 95% CI: 0.403-0.795). Clopidogrel monotherapy was associated with lower risk for MACCE (Kaplan-Meier estimate: 1.0% vs. 3.1%, log-rank p = 0.001 ), as well as lower incidence rates of all-cause death, MI, and stroke. The difference in risk between the groups was statistically similar for major or clinically relevant nonmajor bleeding (Kaplan-Meier estimate: 1.5% vs. 2.1%, log-rank p = 0.199).
Researchers recommended that their findings should be further investigated through a randomized clinical trial.
“Music, community and connection have always played an important role in sacred ceremonies and are an integral component of psychedelic-assisted therapy and integration,” says Payton Nyquvest, Founder and CEO, Numinus. “Through the Music as Medicine by Numinus series, we are celebrating an emerging genre of meditative music and exploring the role that music can play as part of the healing process, while building connection across a community.”
“Psychedelic therapies are moving into legality across the world, and yet it feels like no one is talking about the music that accompanies them,” says Jon Hopkins. “In Indigenous psychedelic ceremonies,” he adds, “the music is as important as the medicine, and has been for thousands of years. Music is how you navigate the space.”
Following the recent announcement of Numinus’ proposed expansion into the U.S., Music As Medicine by Numinus will be hosted in various cities across the U.S. and Canada, celebrating Numinus’ move into the U.S. and reinforcing its community in its home country of Canada. The first event is in Los Angeles on May 21, 2022 at the renowned venue, Lighthouse Immersive, and will consist of five hours of continuous and entrancing live music and visuals by a line-up of the preeminent artists in this emerging genre: Superposition, Justin Boreta, Matthew Davis’ ambient project and East Forest. L.A.-based multimedia art studio Strangeloop, known for their captivating visuals for artists such as Lil NasX, Flying Lotus, and The Weeknd, will be fully enveloping the space with live projection-mapping intended to submerge guests in an all-sensory experience. The event will end with a live, 3D spatial-audio playback of Jon Hopkins‘ most recent, acclaimed album, Music For Psychedelic Therapy, experienced in total darkness, followed by an intimate, live piano performance of “Sit Around the Fire”.
“We are thrilled to be a part of the Music as Medicine by Numinus event series. The intention is to create a safe container for deep listening,” says Justin Boreta. “This is the way this type of music should be experienced.”
“Music to modern humans is like asking a fish what water is. With music more present than ever, I am excited to be fostering spaces that can serve as a spear tip of exploration and experimentation around using music as a tool for inner insight and growth,” says East Forest.
Numinus is also showcasing its Music As Medicine by Numinus concept at DoubleBlind’s Mycelia Festival in Ojai, California, as well as other cities, which will be announced soon.
Tickets for the L.A. event go on sale Friday, April 29 at www.numinus.com/music-as-medicine-event. More information on the other dates will be released in the coming weeks.
About Numinus
Numinus Wellness (TSX: NUMI) helps people to heal and be well through the development and delivery of innovative mental health care and access to safe, evidence-based psychedelic-assisted therapies. The Numinus model – including psychedelic production, research and clinic care – is at the forefront of a transformation aimed at healing rather than managing symptoms for depression, anxiety, trauma, pain and substance use. At Numinus, we are leading the integration of psychedelic-assisted therapies into mainstream clinical practice and building the foundation for a healthier society.
Learn more at www.numinus.com and follow us on LinkedIn, Facebook, Twitter, and Instagram.
Forward-looking statements
This press release contains forward-looking statements within the meaning of applicable securities laws. All statements that are not historical facts, including without limitation, statements regarding future estimates, plans, programs, forecasts, projections, objectives, assumptions, expectations or beliefs regarding future performance are “forward-looking statements”. Forward-looking statements can be identified by the use of words such as “expects”, “does not expect”, “is expected”, “believes”, “intends”, “anticipates”, “does not anticipate”, “believes” or variations of these words, expressions or statements, that certain actions, events or results “may”, “could”, “would”, “might” or “will be” taken, will occur or will be realized. Such forward-looking statements involve risks, uncertainties and other known and unknown factors that could cause actual results, events or developments to differ materially from the results, events or developments expected and expressed or implied in such forward-looking statements. These risks and uncertainties include, but are not limited to, dependence on obtaining and maintaining regulatory approvals, including the acquisition and renewal of federal, provincial, municipal, local or other licenses, and any inability to obtain all necessary government authorizations, licenses and permits to operate and expand the Company’s facilities; regulatory or policy changes such as changes in applicable laws and regulations, including federal and provincial legalization, due to fluctuations in public opinion, industry perception of integrative mental health, including the use of psychedelic-assisted therapy, delays or inefficiencies or any other reason; any other factor or development likely to hamper the growth of the market; the Company’s limited operating and profitability track record; dependence on management; the Company’s need for additional financing and the effects of financial market conditions and other factors on the availability of capital; competition, including that of more established and better funded competitors; the impact of the Russia–Ukraine conflict on the global economy; the continued impact of the COVID-19 pandemic; and the need to build and maintain alliances and partnerships, including with research and development companies, customers and suppliers. These factors should be carefully considered, and readers are cautioned not to place undue reliance on forward-looking statements. Despite the Company’s efforts to identify the main risk factors that could cause actual measures, events or results to differ materially from those described in forward-looking statements, other risk factors may cause measures, events or developments to materially differ from those anticipated, estimated or intended. There can be no assurance that forward-looking statements will prove to be accurate, as actual results and future events could differ materially from those anticipated in forward-looking statements. The Company does not undertake to revise forward-looking statements, even if new information becomes available as a result of future events, new facts or any other reason, except as required by applicable laws.
SOURCE Numinus Wellness Inc.

For further information: Investor Contact: Jamie Kokoska, Vice President, Investor Relations & Communications, [email protected], +1 833-686-4687; Media Contact: Hilary Strath, Director, Communications, [email protected]